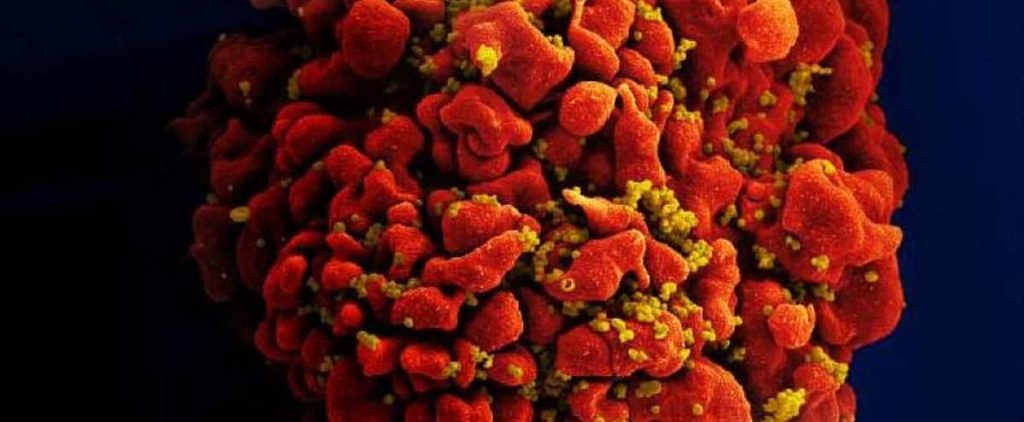
The vaccine, which uses messenger RNA technology, is similar to that found in some Kovid-19 vaccines, but this time against AIDS, the researchers said Thursday, showing promising first results in animals.
Also read: Africa: The fight against HIV has slowed down through COVID-19
Also read: Thanks to Quebec for Curing AIDS
The vaccine has been shown to be safe when given to macaques and the risk of infection from exposure is reduced by 79%. However, it does require improvements before being tested on humans.
“Despite nearly four decades of efforts by the global scientific community, an effective vaccine to prevent HIV remains an elusive goal,” said Anthony Fauzi, co-author of the study and consultant to the House, immunologist Anthony Fawcett. -White on the health crisis.
“This experimental messenger RNA vaccine combines several features that can overcome the failures of other experimental HIV vaccines and thus represent a better approach,” said the director of the U.S. National Institute of Allergy and Infectious Diseases (NIAD).
Scientists at the institute are working with researchers at Modernna, an American company that uses one of the most widely used vaccines against COVID-19.
The study was published Thursday in the prestigious journal Nature.
The vaccine was first tested on mice and then on Rhesus macaws. These received multiple booster doses over a one-year period. Despite the high dose of messenger RNA, the product is well tolerated, causing moderate side effects such as temporary loss of appetite.
At 58E During the week, all macaques developed detectable antibody levels.
From the 60th week onwards, the animals are exposed to the virus every week through the fecal mucosa. Since primates do not cause HIV-1 infection in humans, researchers have used a different, but similar virus, simian HIV (SHIV).
After 13 weeks, only two of the seven immunocompromised macaques survived. But while other vaccinated macaques developed the disease three weeks later, those with immunity took an average of eight weeks.
“This level of risk reduction has a significant impact on viral transmission,” the study said.
The vaccine works by providing genetic clues to the body, causing the formation of two proteins that are characteristic of the virus. These are assembled to form pseudovirus cells (VLPs), mimicking infection to receive an immune system response.
However, scientists have noted that antibody levels are relatively low and that the vaccine, which requires multiple injections, is difficult to administer in humans.
Therefore they want to improve the quality and quantity of VLPs produced before testing the vaccine on humans.





More Stories
Healing Streams Live Healing Services with Pastor Chris: Miracles Await this March 14th – 16th, 2025!
Essential Care for Hermann’s Tortoise: A Guide to Thriving Pets
Nail Decisions: Which is Better for You, Acrylic or Gel?